Anterior Cingulotomy (ACING) for OCD
Table of Contents
ToggleIntroduction
This page provides an overview of Anterior Cingulotomy for OCD. It shares content with the 'Anterior Cingulotomy for depression' pages but provides specific information on outcomes for depression. Some of the text comes from our patient information leaflets on Cingulotomy.
Description of Anterior Cingulotomy
Anterior Cingulotomy (ACING) was initially developed for the treatment of intractable pain (Foltz & White, 1962), but its other indications include anxiety disorders, depressive disorders, and OCD. In recent years, it has become one of the most commonly-used neurosurgical procedures for the treatment of chronic, treatment-refractory depression and OCD.
It is an ablative procedure which involves creating small lesions in a specific part of the brain. The area of the brain that is targeted is the anterior cingulate gyrus. This part of the brain is understood to be involved in some aspects of the regulation of emotion and of automatic bodily responses to events in the world around us. The cingulate gyrus is also involved in some aspects of learning, particularly learning which events in the outside world are pleasant and which are unpleasant.
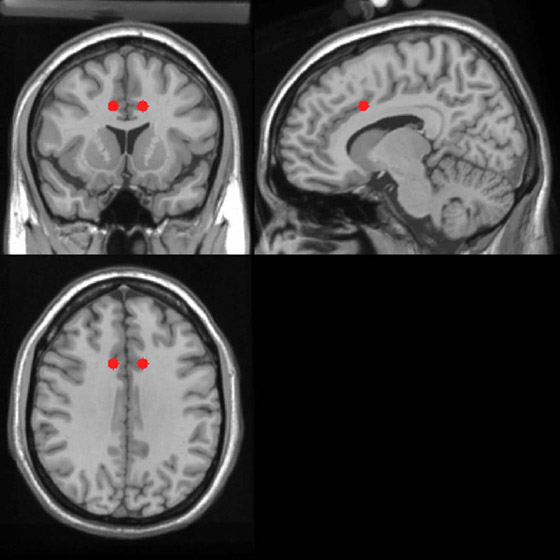
Lesion targets
Cingulotomy lesions target the cingulum bundle within the anterior cingulate gyrus, although lesioning of the bundle is not thought to be essential for clinical benefit. The lesions also involve part of the anterior cingulate cortex. The site of the lesions is shown below in Figure 1.
Neurosurgery in London
For many years now, we have partnered with specialist neurosurgeons at the National Hospital for Neurology and Neurosurgery (NHNN) at Queen Square, London, who perform the surgery. This has been because of a lack of neurosurgeons in Scotland who have experience with 'functional' neurosurgery. Neurosurgeons include Professor Ludvic Zrinzo and Mr Harith Akram (Consultant Neurosurgeon). Admission takes place to the Hughlings Jackson Ward at Queen Square. This is a specialist inpatient ward for neuropsychiatry.
Preparing for surgery
Although patients in Scotland will need to travel to London for the actual surgery, we are alongside them every step of the way. Before they make a decision about proceeding with surgery we will arrange a meeting (usually via MS Teams) with the surgeons in London who can discuss the surgery and answer any questions that people might have.
Travelling to London
If patients need support to travel, nurses from the Advanced Interventions Service are able to accompany the patient to London and assist with the transfer back to Scotland after surgery. The travel will usually be by train, but we will discuss this on a case-by-case basis.
The procedure
Anaesthesia
The operation can be carried out either under local anaesthetic (with the patient awake, similar to a dental procedure) or under a general anaesthetic (with the patient asleep). A frame for the surgery is attached firmly to the patient’s skull, using local anaesthetic to numb the skin and tissue. Unlike skin, bone and other parts of the body, the brain has no sensory nerve supply and cannot ‘feel’ pain.
If the surgery is performed under local anaesthetic, parts of the procedure can be uncomfortable, but it is not painful and your surgeon will guide you at every step. Recovery time is generally quicker under local anaesthetic.
Creation of lesions
The surgery involves the insertion of a 2mm-thin surgical probe into the brain causing a minimum of damage. The probe is guided into position very accurately using a frame that holds the probe and special imaging machines that produce detailed images of the brain: computerised tomography (CT) or magnetic resonance imaging (MRI) scanners. When placed in position by the surgeon, the end of the probe is heated to damage the tissue immediately around the tip. This heat-damaged tissue stops the function of that small part of the brain. This effect is very localised and is permanent.
The operation takes about three hours, although much of this time is taken up by brain scans to locate the correct position for the probes. The surgery itself takes about one hour. The two incisions are usually placed on either side of the top of the patient’s head, around 2 cm from the midline, behind the hairline to hide the scars (although this is not always possible). Most times, no shaving is required at all, but sometimes the scalp around the incisions is shaved. People do not have their whole head shaved.
The scars will eventually fade to a pale line within three to six months and the hair will usually grow back normally if it has been shaved. The skin is closed by a variety of different methods using stitches or skin staples. Stiches or staples are normally removed after about 5-7 days depending on how well the wound has healed.
Outcomes from surgery
The following sections show the clinical outcomes from anterior cingulotomy for patients who underwent surgery for OCD (N=5).
Definitions
The following categorical outcome definitions apply to outcomes from both neurosurgery and intensive treatment. They are similar to those in widespread use (e.g. Mataix-Cols et al, 2016) and recently revisited by Mataix-Cols et al (2022). We have based them around self-report rating scales because these have been used much more widely and scores will be available for more time-points than clinician-rated scales.
- Response is determined by a reduction in Y-BOCS (self-report) score ≥ 35%.
- Partial response is a reduction in Y-BOCS (self-report) score ≥ 25% but less than 35%.
- Remission is a Y-BOCS (self-report) score of ≤ 8.
For the purposes of reporting, ‘response’ and ‘partial response’ are inclusive, and all patients who meet criteria for response will meet criteria for partial response. This is done to provide a meaningful figure to patients when discussing outcomes. For example, it makes more sense to say that 50% of people (for example) will be at least 25% better, and 30% will be at least 50% better.
Baseline demographics
The table below shows the baseline characteristics of patients who have undergone cingulotomy for OCD in Dundee.
| Value | |
| Demographics | |
| N | 5 |
| Sex (M/F) | 4:1 |
| Age (years) | 46.6 ± 11.8 |
| Age (min) | 30.8 |
| Age (max) | 59.8 |
| Illness characteristics | |
| No. of episodes (N) | 1.0 ± 0 |
| Duration of current episode (years) | 28.5 ± 12.2 |
| Age at first episode (years) | 18.3 ± 5.5 |
| At of onset of current MDE (years) | 19.2 ± 6.6 |
| Treatment history | |
| - | - |
| - | - |
| Depressive symptoms | |
| Y-BOCS-CR | 31.6 ± 4.3 |
| Y-BOCS-SR | 32.4 ± 5.7 |
| Quality of Life scores | |
| EQ-5D score | 0.39 ± 0.11 |
| WHODAS score | N/A |
Clinical outcomes
The graph below shows individual outcomes, with response status highlighted by colour.

Categorical outcomes
- The response rate from ACING for OCD as the first procedure is 60.0%.
- The partial response rate is 80.0%.
- The remission rate is 40.0%.
References
Mataix-Cols, D., de la Cruz, L. F., Nordsletten, A. E., et al (2016) Towards an international expert consensus for defining treatment response, remission, recovery and relapse in obsessive-compulsive disorder. World Psychiatry, 15, 80-81. https://doi.org/10.1002/wps.20299
Mataix-Cols, D., Andersson, E., Aspvall, K., et al (2022) Operational Definitions of Treatment Response and Remission in Obsessive-Compulsive Disorder Capture Meaningful Improvements in Everyday Life. Psychotherapy and Psychosomatics, 91, 424-430. https://doi.org/10.1159/000527115
More information
Last Updated on 21 November 2023 by David Christmas
